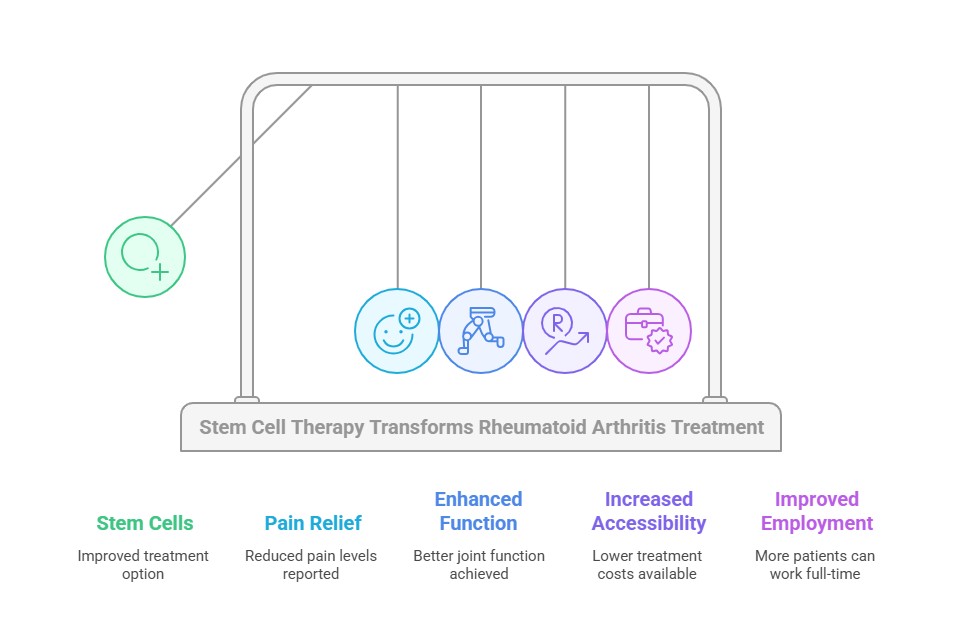
Rheumatoid arthritis affects 5 in every 1000 adults worldwide. Women face a 2-3 times higher risk of developing this debilitating condition. Traditional treatments often don’t work well enough and cause too many side effects. Stem cells for RA now give patients a better chance at lasting relief, offering a potential rheumatoid arthritis breakthrough.
This condition does more than cause physical pain. More than half of patients couldn’t work full-time because of its crippling effects. Recent studies bring good news about stem cell treatment for arthritis. Patients report major improvements in pain levels and joint function that can last months or years. The cost of stem cell therapy for rheumatoid arthritis ranges from USD 5,000 to USD 12,000 in Colombia. Canadian clinics charge $20,000 to $50,000. These lower prices make the treatment available to more patients around the world.


People with rheumatoid arthritis (RA) face unexpected challenges every day. This chronic autoimmune disease disrupts almost every part of daily life and creates obstacles that go way beyond the reach and influence of joint pain.
RA is mainly manifested through constant joint pain—a throbbing, aching feeling that gets worse during rest. The most important symptom is morning stiffness that lasts more than an hour, which makes starting each day tough. As the disease progresses, it damages cartilage that cushions joints and eventually leads to bone erosion.
The physical symptoms hit the same joints on both sides of the body at once. This creates problems all over - studies show all but one of these patients have mobility issues, and only 30% live without pain or discomfort. On top of that, RA patients feel tired 4 to 8 times more often than others.
Basic tasks like getting dressed, cooking, or cleaning need major changes. Many people cut down on standing time, take lots of breaks, or need help with household work.
RA doesn't just hurt the body - it takes a heavy toll on mental health, too. Depression and anxiety strike these patients two to ten times more often than others. Depression makes everything worse by reducing how well patients follow medical advice and leads to more disability and a lower quality of life.
The sort of thing that makes RA so hard to deal with is how symptoms come and go without warning. Patients often talk about feeling tearful, irritable, frustrated, anxious, and depressed. People with RA are eight times more likely to develop a poor body image compared to others.
Life quality drops in many ways: independence, personal strength, and social life. Many patients lose self-esteem, spend less time with others, and worry about money as the disease limits their ability to work.
Current treatments aim to keep disease activity as low as possible, but RA still has no cure. Traditional medications come with big challenges:
Disease-modifying antirheumatic drugs (DMARDs) can slow down the disease but take weeks or months to show results. Joint destruction continues during this waiting time.
TNF inhibitors work well, but 40% of patients don't respond enough to them. About half of those who do respond well at first lose that benefit within just 12 months.
Side effects make treatment even harder. Methotrexate, the go-to DMARD, can cause serious eye problems. TNF antagonists make infections more likely, while corticosteroids bring their own set of tough side effects.
Many patients looking beyond traditional treatments might find new hope in innovative approaches like stem cell therapy for rheumatoid arthritis.
“Stem cells help regulate the immunological system of the body. They can increase regulatory adaptive T cells and decrease inflammatory cells in the peripheral blood, spleen, lymph nodes, and the joints.” — Dr. Neil Riordan, Founder and Chief Scientist at Stem Cell Institute.
Stem cell treatment for rheumatoid arthritis works differently than regular treatments that just mask symptoms. It tackles both inflammation and tissue damage at the same time. This explains why patients often see better results compared to traditional therapies. But can stem cells cure arthritis? While a complete cure is not guaranteed, the treatment shows promising results in managing the condition.
Mesenchymal stem cells (MSCs) have special properties that target the real cause of rheumatoid arthritis instead of hiding symptoms. These cells naturally control the immune system in several ways:
MSCs stop the body from making inflammatory cytokines like TNF-α and IL-6. These are the same molecules that regular RA medicines target, but stem cells do this without side effects. This happens naturally as part of how stem cells work.
These cells also work on many immune system paths at once by:
MSCs create a complete anti-inflammatory environment in affected joints. Research shows that patients who get MSC treatment have much lower levels of key inflammation markers. Their rheumatoid factor drops by 64%, C-reactive protein by 80%, and anti-citrullinated protein antibodies (ACPA) by 71%.
Stem cells offer something unique that regular treatments can't—they help repair damaged joint tissues. MSCs travel directly to inflamed and damaged areas and start their healing work.
Healing happens mainly through paracrine activity. Stem cells release special molecules that help heal nearby tissues. They also release growth factors, cytokines, and exosomes that help cartilage grow back and prevent joints from getting worse.
Studies show that stem cells can help create new cartilage. They might slow down or stop joint destruction because they release substances that fight both inflammation and tissue breakdown.
A study in Regenerative Medicine revealed exciting results. After stem cell treatment, the fixed tissue looked just like healthy cartilage. It became thicker and more flexible - exactly what joints need for cushioning. The stem cells also helped the body make its cartilage cells, which made the healing even better.
This healing power marks a big step forward from regular RA treatments. While old treatments can reduce inflammation, they don't fix joint damage that's already there. Stem cell therapy for joints offers a more comprehensive approach to treating arthritis.


Regencord leads regenerative medicine in Colombia with specialized protocols to treat autoimmune conditions like rheumatoid arthritis. The center has treated more than 5,000 patients worldwide over the last decade, giving hope to patients who have tried everything else without success.
Regencord’s stem cell therapy targets the root cause of rheumatoid arthritis: immune system dysfunction. Their protocols use the immunomodulatory properties of mesenchymal stem cells, which create an environment that reduces harmful immune responses and helps tissue repair.
These specialized treatments have shown impressive clinical improvements by lowering inflammation markers. “One of the autoimmune diseases with greater evidence on benefits and safety of stem cells” describes Regencord’s treatment of rheumatoid arthritis. Their clinical studies show these therapies reduce autoimmune inflammation and help repair damaged tissues.
Regencord's Pereira facility in Colombia offers more than just medical procedures. The team starts with a detailed medical evaluation and creates a customized treatment plan. Their sterile laboratories have specialized equipment and expert staff.
The center stands out because of its focus on patient comfort. Its team stays with patients "throughout the process so that you live a peaceful and satisfying experience." The laboratory follows strict quality and safety standards and has multiple ISO certifications, including ISO 9001, ISO 13022, and ISO 22859.
Regencord's multidisciplinary team includes specialists in:
This scientific group brings over 30 years of experience in regenerative medicine, genetics, biotechnology, and related fields. So, they provide detailed care based on each patient's needs.
The center's excellence shows in its results—90 % of patients got positive results, with zero serious adverse events reported. Patients receive ongoing support through follow-up protocols that track progress and adjust treatments when needed.
Regencord combines scientific excellence with caring support. They offer a real alternative to rheumatoid arthritis patients who haven't found relief through standard treatments.
“Benefits from stem cell treatment for Rheumatoid Arthritis can vary from patient to patient depending on many factors, including current health condition, medical history, level of damage, and other factors.” — Dr. Cesar Amescua, Chief Medical Director at Stem Cell Mexico.
The path from your first consultation to recovery will help you prepare mentally and physically for stem cell therapy for rheumatoid arthritis. Regencord’s step-by-step approach will give a patient the right care at each stage of their treatment experience.
Each patient needs a detailed medical evaluation to determine if they qualify for treatment. This evaluation includes a full review of medical history, current medications, and previous treatments. The specialist also carefully examines how the patient responds to standard treatments.
Doctors usually ask for specific tests from rheumatoid arthritis patients and might need extra diagnostic imaging. This careful screening shows if the treatment will be safe and work for each person. Not everyone can get stem cell therapy. The best candidates are often people who haven't done well with standard treatments or can't take the recommended medications.
After approval, the treatment follows these steps:
This outpatient procedure usually takes 1-2 hours. The medical staff keeps patients comfortable and watched throughout the process.
Medical staff monitors patients for about 4 hours right after treatment. A well-laid-out follow-up plan tracks progress in the days and weeks after. Patients come back for checkups at weeks 1, 4, 8, 12, 26, and 52 after treatment.
Results take time, but many patients see improvements within weeks as stem cells repair damaged tissues. The full benefits become clearer months after the procedure. Based on their clinical evaluation, some patients might need more treatments after 4-6 months.
A healthy lifestyle and following doctor's orders during recovery will improve the effectiveness of the treatment and extend its benefits.


When considering stem cell treatment for RA abroad, smart financial and logistical decisions should come first. Patients must weigh several practical factors beyond the medical benefits we discussed earlier.
Stem cell therapy in Colombia costs between $5,000 and $12,000 USD, which is much lower than in Western countries, where prices for similar procedures reach $25,000 to $50,000 USD. This means patients can save 40-70%.
Traditional RA treatments have significant hidden costs. Around 30-50% of patients don’t respond to conventional DMARDs, which means they need expensive biologic therapies. Long-term medication use also leads to extra expenses from treating side effects and complications.
Colombia stands out as a top destination for stem cell therapy. Major treatment centers operate in Bogotá, Medellín, and Cali. These cities combine world-class medical facilities with great tourism opportunities.
Most clinics that serve international patients provide these services:
People call Medellín the "city of eternal spring" because of its pleasant year-round weather and rich cultural experience. Many facilities put the clinic, hotel, and shopping options under one roof to make things easier for patients.
Patients should get a full picture before moving forward. Here are key questions to ask:
What's the source of stem cells, and how are they processed? What's the medical team's experience with rheumatoid arthritis cases? Does the physician have board certification and special training in regenerative medicine? What happens during post-treatment follow-up? What emergency care is available if complications occur? What improvements can patients expect, and when?
Ask for a detailed treatment plan with clear costs. Check if the facility has proper certifications and participates in IRB-approved research protocols.
Stem cell treatment has become a powerful option for rheumatoid arthritis patients who haven’t found success with regular therapies. Recent research shows that this innovative approach helps reduce pain, improves joint function, and enhances the patient’s quality of life. The benefits last three years or longer, and patients show lower levels of inflammatory markers.
Regencord’s team of medical experts uses specialized protocols at its modern facilities in Colombia. It gives patients a complete treatment experience that costs much less than in North America. Its results prove its success—it’s treated over 5,000 patients worldwide, with 90% reporting positive outcomes.
Patients need to consider practical details like travel plans and treatment costs. Still, many find it worth the investment compared to spending years on conventional treatments. These patients have regained their mobility and returned to challenging careers.
This therapy has become more than just another treatment choice—it gives hope to people looking for lasting relief from rheumatoid arthritis. The combination of careful patient screening, tailored treatment plans, and committed follow-up care helps reshape the scene of regenerative medicine while changing patients’ lives.
3-Step Process for Stem Cell Treatment for Arthritis in Hands
Stem cells are unique cells with the ability to develop into various cell types and repair damaged tissues. They are used in regenerative medicine, including treatments for cancer, neurodegenerative diseases, and injuries. Sources include bone marrow, cord blood, and embryos.
(888) 540-4101
Begin your journey with us today! Call us at (888) 540-4101 or complete the form to learn more.


