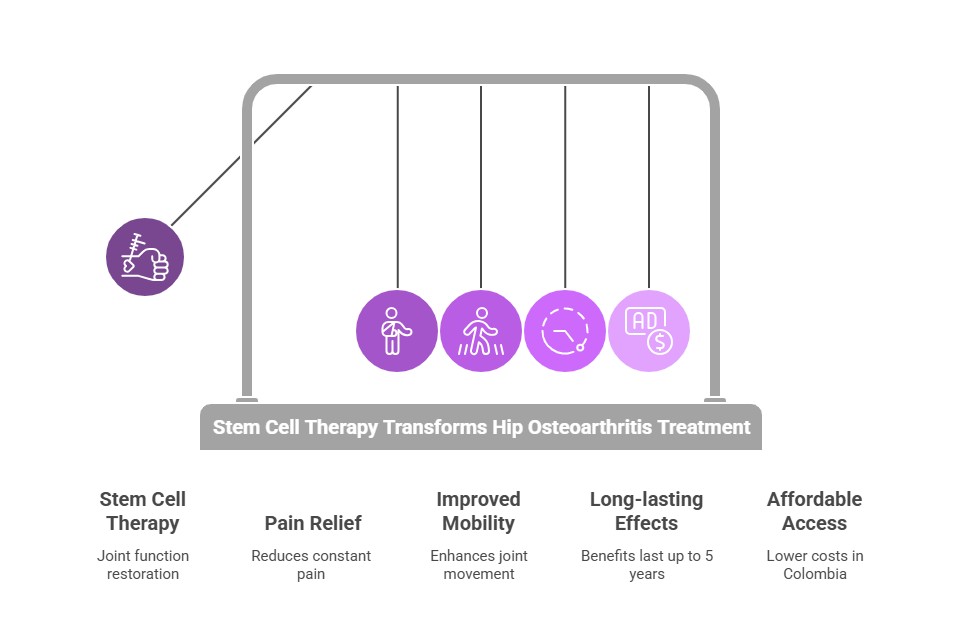
Hip osteoarthritis impacts millions worldwide. People with this condition deal with constant pain, stiffness, and mobility issues. Medications and surgery provide short-term relief, but stem cells for hips have emerged as a game-changing solution, with success rates reaching 70-80%.
Stem cell therapy offers pain relief and better joint mobility that lasts up to 5 years. The treatment helps repair damaged cartilage and reduces inflammation by introducing mesenchymal stem cells into the affected joint. Colombian clinics charge $3,000 to $7,000 for this procedure – nowhere near the prices in the United States or Canada.
This makes regenerative medicine for hips available to many patients with hip conditions like hip dysplasia and AVN.
This piece shows how stem cell therapy helps restore joint function. You'll learn about Regencord's treatment process and what your recovery from a stem cell injection in your hip might look like.

Millions of people worldwide face daily challenges from hip osteoarthritis. This degenerative joint condition affects older adults more than any other group and ranks as the most common type of arthritis. It causes lasting pain and disability. People’s daily routines change as their condition gets worse.
Hip osteoarthritis shows several distinct symptoms that develop over time. Pain stands out as the most common sign, usually starting in the groin area but spreading to the thigh, buttocks, or knee. Patients experience these symptoms as the condition advances:
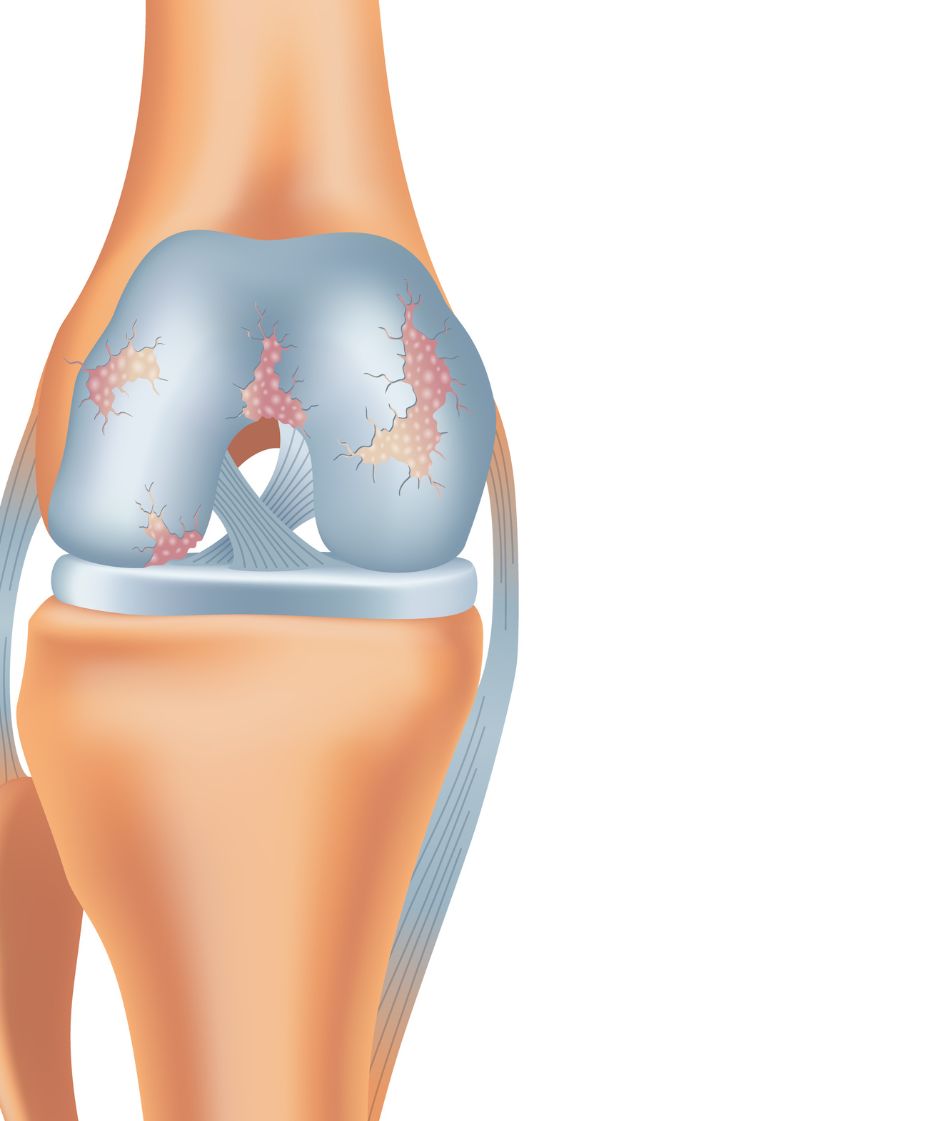
Most patients notice their symptoms start slowly and get worse over months or years. The pain pattern changes as the disease progresses. It first appears during activity and later shows up during rest and at night. Cartilage breaks down and causes bone-to-bone contact, inflammation, and bone spurs (osteophytes) to form.
These conditions affect the hip joint differently. Hip dysplasia occurs when the hip socket (acetabulum) doesn't cover enough of the femoral head due to structural problems. Hip osteoarthritis, on the other hand, breaks down normal joint cartilage.
Hip dysplasia raises the risk of developing osteoarthritis. Research shows it causes 5-10% of all hip osteoarthritis cases in the United States. Women under fifty most commonly develop hip arthritis from hip dysplasia.
These conditions share an important link. Severe hip dysplasia patients (with LCEA ≤18°) face a much higher chance of developing hip osteoarthritis. Higher body mass index (>29) and older age when symptoms start also raise this risk substantially.
Hip osteoarthritis treatments focus on managing symptoms rather than stopping disease progression, despite how common it is. No drugs can prevent or slow down osteoarthritis. This creates a major gap in treatment options.
Standard treatment starts with acetaminophen (up to 4,000 mg daily). Doctors prescribe nonsteroidal anti-inflammatory drugs (NSAIDs) when pain gets worse. These medications carry serious risks, especially for elderly patients:
When medications don't work, patients try intra-articular injections of glucocorticoids. These shots don't work as well in hip joints as they do in other joints. Many patients end up needing arthroplasty (joint replacement). While this solution proves economical, patients endure "a long trajectory of pain and functional limitation" and risk other complications.
Stem cell therapy is a groundbreaking way to treat hip joint degeneration. It gives hope to patients who want alternatives to traditional treatments. This innovative procedure uses the body’s natural healing abilities and could provide long-lasting relief for people with deteriorating hip joints.
Stem cell therapy for hip osteoarthritis uses the regenerative potential of mesenchymal stem cells (MSCs). These remarkable cells can transform into various cell types, including chondrocytes (cartilage cells), osteoblasts (bone cells), and myocytes (muscle cells).
MSCs help repair cartilage in several ways:
Osteoarthritis disrupts the balance between tissue breakdown and repair in joints. MSCs help restore this balance by reducing inflammation and stimulating natural healing. They convert pro-inflammatory M1 macrophages into healing-promoting M2 macrophages that produce anti-inflammatory cytokines vital for tissue repair.
Regencord uses several sources of stem cells that each offer unique benefits for treating hip conditions:
Bone marrow-derived stem cells: Doctors collect these cells from the patient's iliac crest (pelvic bone) using local anesthesia. Research shows they work well for treating orthopedic conditions. Physicians can extract these cells, combine them with platelets and white blood cells, and inject them directly into damaged hip tissue.
Adipose-derived stem cells: These cells come from abdominal fat tissue and are a rich source of MSCs with natural anti-inflammatory properties. Studies show that adipose-derived MSCs have more regenerative cells than bone marrow aspirate concentrate (BMAC). Doctors can collect them through simpler procedures. One study showed significant improvements in patients with early hip osteoarthritis who received adipose-derived MSC treatment with no adverse effects.
Using a patient's stem cells (autologous treatment) reduces the risk of rejection or infection. Both treatments can be done as outpatient procedures with minimal recovery time.
Stem cells start a complex healing process in several stages after entering the hip joint:
The cells first release cytokines that reduce inflammation and create conditions for repair. Because of this anti-inflammatory effect, patients often feel less pain within weeks of treatment.
Stem cells then begin to influence tissue regeneration through multiple pathways. They either become cartilage cells directly or encourage existing cells to repair damaged tissue through paracrine effects.
This regenerative process continues over time. Pain and mobility usually improve within 2-6 weeks after treatment. The full benefits develop gradually, and joint function keeps improving over several months. Research has shown that within a year, patient-derived new cartilage tissue significantly fills cartilage defects.
Yes, it is a natural approach to healing that could be a promising alternative to stem cell hip replacement. Many patients might delay or avoid more invasive procedures.

Regencord’s healing process starts with a full picture of your condition. Each patient gets customized care that continues from the first consultation until treatment ends.
Regencord specialists perform a complete evaluation to determine if stem cells for hip arthritis suit your condition. Patients qualify when they show functional and radiological signs of hip osteoarthritis. Their pain levels should exceed 40 on the Visual Analogue Scale (100mm), and conventional treatments like analgesics or injections should have failed.
Some conditions might make you ineligible:
Doctors watch your body's movement and use ultrasound to analyze hip function with up-to-the-minute data. This gives them a better understanding of pain sources and functional limitations.
Regencord's team of specialists creates a customized plan based on your specific condition. They review your medical history, imaging studies (X-rays, MRI), and laboratory tests to check if you qualify.
Your treatment plan covers the whole process. It includes required treatment numbers, stem cell sources, administration methods, and expected outcomes. To name just one example, some patients receive the Regencord SD Injectate (a patented protocol using bone marrow concentrate containing stem cells), while others benefit from specialized PRP formulations.
The bone marrow aspiration procedure happens on treatment day, usually from your posterior iliac crest (pelvic bone). The medical team sterilizes the area and uses local anesthesia for your comfort.
Your physician extracts about 30 ml of bone marrow (or 60 ml for treatments on both sides) with a specialized needle. A centrifuge processes this bone marrow aspirate right away to isolate and concentrate stem cells before injection.
Advanced imaging guides the precise stem cell injection for the hip. Regencord's technique will perfectly place cells where you need them most. Each intra-articular injection delivers about 20 million expanded stem cells.
The medical team provides specific care instructions after your procedure. You should avoid anti-inflammatory medications for at least six weeks because they can interfere with healing. They recommend:
Stem cell therapy is an outpatient procedure. You can go home the same day and return to normal activities within 2-3 days with some movement restrictions. Regular check-ups help monitor your progress and allow treatment adjustments when needed.
The recovery experience after stem cell treatment follows a predictable pattern. This helps patients create realistic expectations about their healing process. A clear understanding of the timeline allows patients to balance rest and activity for the best results from their stem cell treatment for hips.
The original treatment site becomes sore for 48-72 hours, depending on each patient’s pain tolerance. The anti-inflammatory benefits of stem cells help many patients experience less pain during the first week. Most patients return to their normal condition within seven days after the injection.
This vital period requires patients to
Pain levels and mobility start showing noticeable improvements as time progresses. Pain reduction and functional improvements become evident between 2 and 6 weeks after treatment. During this time, stem cells begin repairing and regenerating damaged tissue.
Most patients can resume walking and cardio activities by weeks 3-4. Healthcare providers may approve weightlifting and running after about four weeks. Physical therapy remains essential through this phase. The exercises boost blood flow to treated areas and speed up tissue repair.
Patients see continuous improvement across several measures. Research shows significant enhancements in standardized assessments:
Male patients show better functional outcomes, with improvements of 12.27% compared to 5.23% in females one year after treatment. These benefits continue developing between 3 and 6 months after the procedure when stem cells reach peak potency.
Studies show promising results. All but one of six studies on stem cell treatment for hip osteoarthritis reported significant improvement in patient-reported outcomes. Multiple studies confirm an excellent safety profile with no major complications.
Stem cell therapy is a proven solution for patients with hip osteoarthritis. It provides major pain relief and better mobility, lasting up to 5 years. Research consistently shows positive outcomes. Many studies reveal substantial improvements in pain scores and functional assessments. Patient stories verify these findings, with remarkable recoveries as patients return to activities they love.
Traditional treatments manage symptoms only. Stem cell therapy tackles the root cause of natural regeneration. This method gives lasting results without the risks of major surgery. Specialized facilities like Regencord make this treatment accessible. The lower cost compared to standard options makes it an appealing choice for many patients.
The success rate of stem cell therapy for hips reaching 70-80% makes it a leading treatment for hip osteoarthritis. Recovery time is minimal, with few complications. Patients looking for long-term solutions to hip pain receive complete care. The process includes detailed evaluations, individual-specific treatment plans, and dedicated follow-up support.
We focus on knee treatment using stem cell therapy, focusing on three main processes:
Stem cells are unique cells with the ability to develop into various cell types and repair damaged tissues. They are used in regenerative medicine, including treatments for cancer, neurodegenerative diseases, and injuries. Sources include bone marrow, cord blood, and embryos.
(888) 540-4101
Begin your journey with us today! Call us at (888) 540-4101 or complete the form to learn more.


